Diverticulitis: The excruciating bowel disease that may be out to get us
09
July
2021
What is behind this common disease?
As we get older, the chances of developing diverticulitis are greater.
Diverticulitis is a frequent but confusing condition that affects the large intestine (bowel). So why don't we take small steps and learn about this curious condition from the beginning? How does it happen? Who does it affect? Is it as painful as it sounds?
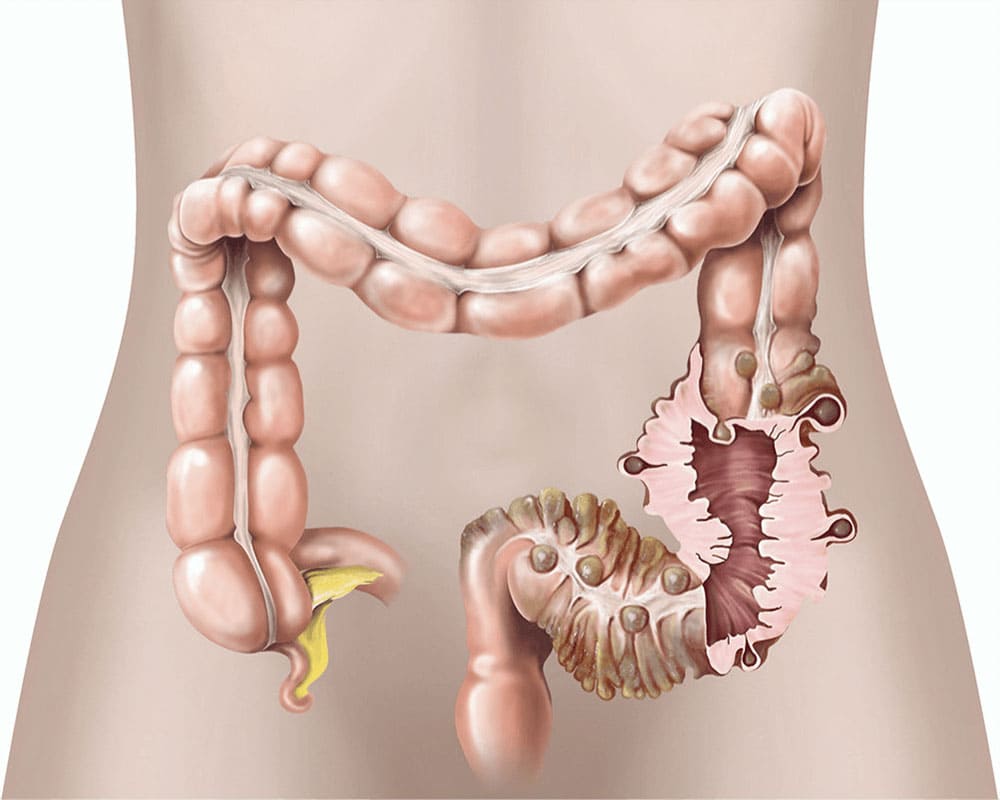
Diverticula are little bulges or pockets that can form in the intestine's lining as you age. The majority of patients with diverticula do not experience any symptoms and are only diagnosed after undergoing a scan for another reason. When the patient has no symptoms, the condition is called diverticulosis. However, it is called diverticular disease when the diverticula creates symptoms such as pain in the lower belly. In addition, when the diverticula becomes inflamed or infected, it results in more severe symptoms (excruciating lower abdominal cramps). It is then called diverticulitis, which might manifest as an acute or chronic condition. Diverticulitis is considered the most serious type of divacular disease.
In some cases, it can cause serious complications and occurs in 10% to 25% of patients. If left unchecked, they can lead to long-term health issues. Based on that information, you might want to take it seriously.
What causes diverticulitis?
Although the reasons for diverticulitis and diverticular disease may not be 100% accurate, research has narrowed it down to three main ones: age, lifestyle and diet, and genetics.
Age: The walls of your large intestine weaken as you become older, and the pressure of hard stools traveling through your intestines might induce diverticula. By the age of 80, the vast majority of people will have some form of diverticula.
Lifestyle and diet: Doctors suggest that diverticular disease and diverticulitis are related to a lack of fiber in the diet. Fiber helps to soften and expand your stool, reducing strain on the walls of your intestines. Other factors that appear to raise your risk include:
Smoking: Diverticular disease, including diverticulitis, is more common among smokers than in nonsmokers.
Obesity or being overweight: Diverticulitis is more common in those with a higher BMI and wider waistlines, according to several studies.
Obesity may increase the risk of diverticulitis by altering the bacterial balance in your gut, but more research is needed to understand the impact this plays entirely.
Vitamin D: According to a study, those with higher vitamin D levels may have a lower risk of developing diverticulitis. To fully comprehend the probable link between vitamin D and this illness, more research is required.
Having a constipation history.
Excessive use of painkillers and nonsteroidal anti-inflammatory drugs, such as ibuprofen and aspirin, may increase the risk of developing diverticulitis.
Genetics: If you have a close family relative who has a diverticular disease, especially if they had it before the age of 50, you're more likely to have it as well, but let's keep our fingers crossed!
What are possible symptoms?
Symptoms of diverticulitis can range from minor to severe. These signs and symptoms might arise quickly or build over several days. In addition, diverticular illness can cause the following symptoms:
Abdominal discomfort that commonly occurs in your lower left side and is worse while or shortly after eating (evacuating feces or passing gas ease it)
Bloating
Diarrhea, constipation, or both
Occasionally, blood in your stool.
If you have diverticulitis, you may have the following symptoms:
Abdominal discomfort that is persistent or severe
Nausea and vomiting, as well as a fever and chills
Mucus or blood from your rectum or in your stool
When to call the doctor?
The most frequent symptom of diverticulitis is abdominal pain. As mentioned before, it will most likely happen on your lower left side of the abdomen. It can, however, appear on the right side of your tummy.
If you develop diverticular disease or diverticulitis symptoms, you should see your doctor as soon as possible. However, if you've already been diagnosed with diverticular disease, you won't need to see a doctor because the symptoms can usually be handled at home.
However, if you have any of the symptoms listed above, such as vomiting or blood in your stool, it could indicate a significant complication from diverticulitis or another condition. So book an appointment with your doctor right away.
Complicated and uncomplicated diverticulitis
Your doctor can determine whether your diverticulitis is complicated or not. More than 75% of diverticulitis cases are uncomplicated, leaving just around 25% of patients with complex symptoms.
Complications may include:
Fistula, which is an irregular connection that can form between two organs or between an organ and the skin
Abscess, a pus-filled infected pocket.
Phlegmon, a kind of infection that is less well-contained than an abscess.
Fistula, a developed abnormal connection between two organs or between an organ and the skin
Intestinal perforation, a rip or hole in the intestinal wall that allows colon contents to seep into the abdominal cavity, causing irritation and infection.
intestinal obstruction, a blockage in your intestine that can prevent feces from passing
Diagnosing diverticulitis
Your doctor will most likely ask you about your symptoms, medical history, and any drugs you're taking to diagnose diverticulitis. Then, they'll probably do a physical exam to check for tenderness in your abdomen or, if more information is needed, a digital rectal exam to look for rectal bleeding, pain, lumps, or other issues.
A variety of different illnesses can cause diverticulitis-like symptoms. Your doctor may conduct one or more tests to rule out other diseases and look for evidence of diverticulitis. Tests may include:
Abdominal ultrasound, abdominal CT scan, abdominal MRI scan, or abdominal X-ray for the gastrointestinal (GI) tract
Colonoscopy to inspect the inside of the GI tract
Stool test to check for infections, such as Clostridium difficile
Urine test to check for infections
Blood tests to look for symptoms of inflammation, anemia, or problems with the kidneys or liver
Pelvic check for women to rule out gynecological issues
A pregnancy test is used to rule out pregnancy
Treating diverticulitis
Depending on the severity of the complications, your doctor will determine adequate treatment. Diverticulitis that is not complicated may usually be managed at home. Your doctor could advise you to make dietary adjustments. In some situations, they may give antibiotics as well as other medicines, and maybe surgery.
Diet
Your doctor may recommend avoiding solid foods and adopting a clear-liquid diet for a few days to allow your digestive system to rest and heal. If your symptoms are minor or have begun to improve, you might try eating low-fiber meals until your condition improves. Once the symptoms have stopped, you can resume a higher-fiber diet, aiming for 30 grams of fiber per day.
-
Medicine
Doctors usually recommend antibiotics, which are generally enough to cure diverticulitis at home. They include metronidazole (Flagyl, Flagyl ER), amoxicillin, and moxifloxacin.
To relieve pain, you can use paracetamol; however, if it isn't helping, you should see a doctor. Avoid taking aspirin and ibuprofen because they might irritate your stomach, so it's best to stay away.
If your case of diverticulitis is more severe, it may require hospitalization. You'll probably have antibiotic shots in the hospital, and a tube directly linked to your vein will keep you hydrated and fed (intravenous drip). If paracetamol isn't working, a more potent painkiller may be recommended.
-
Surgery
It is usually rare, but surgery may be required in certain cases to address significant complications of diverticulitis. The damaged portion of your large intestine is generally removed during surgery. Colectomy is the medical term for this procedure, and it is the treatment for uncommon problems, including fistulas, peritonitis, or intestinal obstruction. You may have a temporary or permanent colostomy after a colectomy, in which one end of your intestine is redirected via a hole in your stomach. Percutaneous drainage is another procedure used for abscesses, which are the most prevalent complication of diverticulitis. Again, a radiologist performs the surgery.
Home remedies and prevention
Although home remedies generally consist of diet changes, you might consider few other options to prevent diverticulitis and improve your digestive health in general.
Certain types of probiotics have been reported to help alleviate or prevent symptoms of diverticulitis in several trials. However, more study is needed to assess the possible advantages and risks of utilizing probiotics to treat diverticulitis.
Certain herbs or supplements may be beneficial to your digestive health as well. However, there isn't much evidence to back up the usage of herbal treatments right now.
It also might help to follow these lifestyle changes; for instance, it could be beneficial to:
keep a healthy body weight
Limit your intake of saturated fat
Acquire adequate vitamin D
Follow a high-fiber diet
Exercise on a regular basis
Avoid smoking cigarettes and anything else
These preventative measures may be an act of prevention toward diverticulitis, but if you follow and stick to them, they can also aid in promoting excellent overall health. So why not live on the healthy track?
If you or anyone you know is suffering from pain, call us today on (254) 580-8765 to book an appointment with our expert doctors.