Nociceptive pain
10
July
2021
Understanding Nociceptive Pain
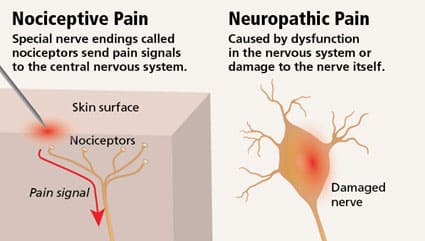
As much as we hate to be in pain, we’ve got to be grateful for it as being a significant communicator between the body and brain. Imagine the consequence of not feeling pain when walking on hot coal, for instance. In a way, pain is the body’s cry for help for a condition or cause in dire need of attention and care. Despite people’s different experiences with pain, it can be categorized into two main types based on the kind of damage done. Neuropathic pain is caused by nerve damage while nociceptive pain is due to tissue damage. Nociceptive pain is today’s topic of discussion.
Nociceptive pain is considered as the most common type of pain that stems from the injury of a tissue. It is caused by the detection of noxious or potentially harmful stimuli by the nociceptors. For instance, the injury can be to the bone, skin, muscles and other tissues. Injuries to the body tissue can be internal from a disease such as cancer, or external due to a physical injury such as a cut, bruise or a broken bone.
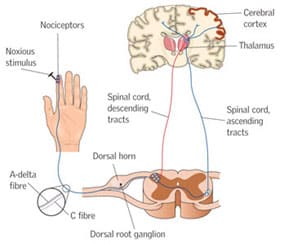
Nociceptors are pain receptors that are stimulated by chemical, physical or thermal stimuli that may harm the body’s tissues. Once activated, electrical signals are sent to the central nervous system by the receptors which then causes the sensation of pain.
Types of Pain:
Nociceptive pain can either be acute or chronic. For instance, acute pain caused by the damage of the soft tissues can result from physical or soft injuries such as a sprained ankle. Although, it is sharp in nature, yet it goes away as soon as its underlying cause is healed. Chronic pain, on the other hand, is a continuous pain and usually lasts for longer than six months. It may even last even after the healing of an injury or illness, for pain signals remain active for a longer period of time. It is also important to note that some people suffer from chronic pain in the absence of a past injury or apparent body damage. In this case, it can be linked to a variety of conditions such as arthritis, headache, cancer, nerve pain, back pain and fibromyalgia (widespread pain).
In addition to that, nociceptive pain can be further classified into visceral pain, somatic pain and radicular pain.
1- Visceral Pain
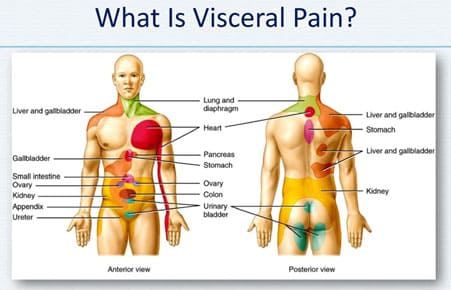
Visceral pain can be felt when the pain receptors of or near the internal organs such as the pelvis, abdomen, chest or intestines are activated after an injury or damage caused to an internal organ. Its location is considered vague as it is often hard to pinpoint the exact location of visceral pain.
Symptoms:
Visceral pain is often linked with:
-
Pressure
-
Aching
-
Squeezing
-
Cramping
Moreover, other symptoms reported include:
Nausea or vomiting
Changes in body temperature
Heart rate
Blood pressure
Causes:
As previously mentioned, it is felt after the damage, injury or inflammation of an internal organ such as:
Injuries to the gallbladder, intestines, bladder or kidneys (gallstone – irritable bowl syndrome)
Damage of the core muscles or abdominal wall
Spasms in the core muscles
Acid indigestion
Digestive problems such as constipation
Infections in the digestive and renal systems
Problems in the pancreas or liver
Cancer that affects internal organs such as stomach cancer
Endometriosis
Menstrual pain
Prostate damage
Appendicitis
2- Somatic Pain
Somatic nociceptive pain originates from the activation of nociceptors in the skin, bones, connective tissue, muscles or joints. It is often stimulated by movement, temperature or swelling, and can be described as sharp in nature. It is also well localized in initial stages, in opposition to visceral pain. However, it can spread across larger areas of the body depending on the extent of the injury. It may also progress into a dull ache with time especially for deep somatic pain in the muscles and bones.
Symptoms:
This type of pain is often associated with:
cramping
gnawing
aching
sharp pain
Types of somatic pain:
Somatic pain is often divided into two categories: superficial pain and deep somatic pain.
Superficial Pain:
It occurs when the pain receptors in the skin, mucus and mucous membranes are activated. Common, everyday injuries usually cause superficial somatic pain.
Deep Somatic Pain:
Deep somatic pain occurs when the stimuli activate pain receptors deeper in the body such as in tendons, joints, bones and muscles. Deep somatic pain is usually associated “aching” than the superficial somatic pain.
Causes:
Given that somatic pain arises from a variety of sources, it has many different potential causes such as:
A small or large injury to joints or bones
A trauma or cut to the skin
A fall that damages the connective tissues
A strained muscle due to excessive use
A bone fracture
Diseases that affect connective tissues such as osteoporosis
Cancers that affect the bones and skin
Arthritis that leads to swelling of the joints
Diagnosing Visceral and Somatic pains:
Both somatic and visceral pain are expected to subside within a few days. However, in case of severe or persistent week for at least week, it is advised to consult a doctor. The patient will be asked about the symptoms, location of the pain, intensity of the pain, how often it occurs, medical history and what affects it. In addition to that, the doctor might request run objective tests such as lab analyses and physical exams. Once a diagnosis is established, the doctor will set a treatment plan. The treatment differs according to the underlying cause. For instance, if it is caused by a joint pain, you’d be referred to an orthopedist, or to a gastroenterologist in case of a stomach issue.
Treatment:
Given the subjectivity and varying experience of pain, treatment can get tricky.
Treating somatic pain:
Medicines, either over-the-counter medicines or prescription medications, are often prescribed to treat somatic pain. However, when it comes to medicines, it is always important to responsibly deal with them as some are highly addictive. Injections might be also used to treat the joints and bones, and are often requested by orthopedists and rheumatologists.
Treating visceral pain:
Pain-reliving drugs are sometimes used to treat visceral pain. However, since visceral pain is less localized and more spread out in the body, it is harder to prescribe the exact medication that will help. As researchers learn more about visceral pain, new methods are being developed to treat it.
Lifestyle changes:
At times, traditional treatment plans that include medication and treating the underlying source of pain is not quite enough nor the only way to manage the symptoms of pain. Consequently, lifestyle changes are often coupled with the traditional treatment plan for better results. Lifestyle changes include:
-
Opting for relaxing activities
-
Good nutrition, especially for visceral pain
-
Meditation such as yoga
-
Tai chi, an ancient Chinese tradition, considered as a graceful form of exercise. It includes a series of slow movement practiced in a focused manner and deep breathing.
-
TPhysical therapy to strengthen and stretch the affected muscles or joints
-
Keeping a journal where you can express your thoughts
-
Low-impact exercises, such as swimming and walking
-
High-intensity exercise (with reasonable limits) such as tabata training
-
Behavioral therapy
-
Getting enough sleep
-
Reducing or stopping smoking and drinking
-
Acupuncture (with mixed evidence) which is an alternative form in medicine and a main component in traditional Chinese medicine. It is the process of penetrating thin, solid and metallic needles into the skin.
-
Osteopathic manipulation therapy (OMT) that helps in correcting structural imbalances in the body, improve circulation and relieve pain.
However, it is important to consult a doctor before engaging in any of the above activities, for some would cause more damage. For example, some exercises can be harmful for knee pain.
Outlook
It is widely circulated that one can’t enjoy nor appreciate pleasure without pain. The first step towards a healthy pleasure life is the person himself, and next comes the doctor that provides the most suitable treatment. On the other side of the token, not being able to feel pain is far from being lucky, for it hints at an underlying condition as well. Moral of the story; pain is a blessing in disguise, more or less.
References:
Duggal, Neel. “Somatic Pain vs. Visceral Pain”. Healthline
Retrieved from :
https://www.healthline.com/health/somatic-vs-visceral-pain
Franks, Ian. “Nociceptive Pain”. Healthline.
Retrieved from :
https://www.healthline.com/health/nociceptive-pain
Pharm, Yolanda. “What is Nociceptive Pain?”. News Medical Life Sciences.
Retrieved from :
https://www.news-medical.net/health/What-is-Nociceptive-Pain.aspx
Santons-Longhurst, Adrienne. “Types of Pain: How to Recognize and Talk About Them”. Healthline
Retrieved from :
https://www.healthline.com/health/types-of-pain
If you or anyone you know is suffering from pain, call us today on (469) 562 4188 to book an appointment with our expert doctors.