Colonoscopy Procedure
23
Sep
2021
What is a Colonoscopy?
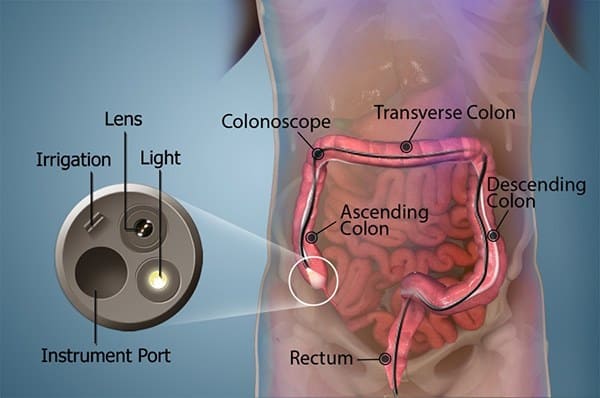
A colonoscopy is an examination used to find out changes or deformities in the large intestine (colon) and rectum.
At the time of the colonoscopy, a long, flexible tube (colonoscope) is inserted into the rectum. A small video camera at the tip of the tube enables the doctor to view the inside of the entire colon.
If required, polyps or other types of abnormal tissue could be removed through the scope during a colonoscopy. Tissue samples (biopsies) could be taken during a colonoscopy as well.

Why it is done
Your doctor might recommend a colonoscopy to:
- Investigate intestinal signs and symptoms - A colonoscopy could help your doctor explore possible causes of abdominal pain, rectal bleeding, chronic constipation, chronic diarrhea, and other intestinal problems.
- Screen for colon cancer - If you are 50 years or older and at average risk of colon cancer and have no colon cancer risk factors other than age, your doctor might recommend a colonoscopy every ten years or sometimes sooner to screen for colon cancer. Colonoscopy is one alternative for colon cancer screening. Talk with your doctor about your options.
- Look for more polyps - If you have had polyps before, your doctor might recommend a follow-up colonoscopy to look for and remove any additional polyps. This is done to lower your risk of colon cancer.
Colonoscopy Risks
A colonoscopy poses some risks. Rarely, complications of a colonoscopy might include:
- Adverse reaction to the sedative used at the time of the examination
- Bleeding from the area where a tissue sample (biopsy) was taken or a polyp or other abnormal tissue was removed
- Tear of the colon or rectum wall (perforation)
After discussing the risks of colonoscopy with you, your doctor will ask you to sign a consent form authorizing the procedure.
Colonoscopy Preparation
Before a colonoscopy, you will be required to clean out (empty) your colon. Any residue in your colon might block the view of your colon and rectum during the examination.

To empty your colon, your doctor might ask you to:
- Follow a special diet the day before the examination - Generally, you would not be able to eat solid food the day before the examination. Drinks might be limited to clear liquids such as plain water, tea, and coffee without milk or cream, broth, and carbonated beverages. Avoid red liquids, which could be confused with blood during the colonoscopy. You might not be able to eat or drink anything after midnight the night before the examination.
- Take a laxative - Your doctor will generally recommend taking a laxative, in either pill form or liquid form. You might be instructed to take the laxative the night before your colonoscopy, or you might be asked to use the laxative both the night before and the morning of the procedure.
- Use an enema kit - Sometimes, you might need to use an over-the-counter enema kit either the night before the examination or a few hours before the examination to empty your colon. This is generally only effective in emptying the lower colon and is often not recommended as the main way of emptying your colon.
- Adjust your medications - Remind your doctor of your medications at least a week before the examination particularly if you have diabetes, high blood pressure, or heart problems or if you take medications or supplements that consist of iron.
Also tell your doctor if you take aspirin or other medications that thin the blood, like warfarin (Coumadin, Jantoven), newer anticoagulants, like dabigatran (Pradaxa) or rivaroxaban (Xarelto), used to lower the risk of blot clots or stroke - or heart medications that affect platelets, like clopidogrel (Plavix).
You might need to adjust your dosages or stop taking the medications momentarily.
What you can expect
During the procedure
At the time of the colonoscopy, you will wear a gown, but likely nothing else. Sedation is generally recommended. In some cases, a mild sedative is given in pill form. In other cases, the sedative is combined with an intravenous (IV) pain medication to reduce any discomfort.
You will start the examination lying on your side on the examination table, generally with your knees drawn toward your chest. The doctor will insert a colonoscope into your rectum.
The scope which is long enough to reach the full length of your colon contains a light and a tube (channel) that allows the doctor to pump air or carbon dioxide into your colon. The air or carbon dioxide inflates the colon, which offers a better view of the lining of the colon.
When the scope is moved or air is introduced, you might feel abdominal cramping or the need to have a bowel movement.
The colonoscope also consists of a small video camera at its tip. The camera transmits or sends pictures to an external monitor so that the doctor could study the interior of your colon.
The doctor could also insert instruments through the channel to take tissue specimens (biopsies) or remove polyps or other regions of abnormal tissue.
A colonoscopy generally takes about thirty to sixty minutes.
After the procedure
After the examination, it takes about an hour to start to recover from the sedative. You will need someone to take you home because it could take up to a day for the full effects of the sedative to wear off. Do not drive or make crucial decisions or go back to work for the rest of the day.
If your doctor removed a polyp during your colonoscopy, you might be advised to eat a special diet momentarily.
You might feel bloated or pass the gas for several hours after the examination, as you clear the air from your colon. Walking might help relieve any discomfort.
You might also observe a small amount of blood with your first bowel movement after the examination. Generally, this is not a cause for alarm. Consult your doctor if you continue to pass blood or blood clots or if you have continuous stomach pain or a fever. While unlikely, this might happen immediately or in the first few days after the procedure, but might be postponed for up to 1 to 2 weeks.
Colonoscopy Results
Your doctor will check the results of the colonoscopy and then share the results with you.
Negative result
A colonoscopy is considered negative if the doctor does not find any abnormalities in the colon.
Your doctor might recommend that you have another colonoscopy:
- In 10 years, if you are at medium risk of colon cancer you have no colon cancer risk factors other than age
- In 5 years, if you have a history of polyps in previous colonoscopy procedures
- In 1 year, if there was a residual stool in the colon that prevented a complete exam of your colon
Positive result
A colonoscopy is considered positive if the doctor finds any polyps or unusual tissue in the colon.
While most polyps are not cancerous, some could be pre-cancerous. Polyps removed during colonoscopy are sent to a lab for analysis to determine whether they are cancerous, pre-cancerous, or non-cancerous.
Depending upon the size and number of polyps, you might need to follow a more rigorous surveillance schedule in the future to look for additional and/or new polyps.
If your doctor encounters one or two polyps less than 0.4 inches (1 centimeter) in diameter, he or she might recommend a repeat colonoscopy in 5 to 10 years, depending upon your other risk factors for colon cancer.

Your doctor will recommend an earlier colonoscopy if you have:
- More than two polyps
- A large polyp larger than 0.4 inches (1 centimeter)
- Polyps and also residual stool in the colon that prevents complete exam of the colon
- Polyps with specific cell characteristics that indicate a higher risk of future cancer
- Cancerous polyps
If you have a polyp or other abnormal tissue that could not be removed during the colonoscopy, your doctor might recommend a repeat exam with a gastroenterologist who has special expertise in the removal of large polyps, or surgery.
Problems with your examination
If your doctor is concerned about the quality of the view through the scope, he or she might recommend a repeat colonoscopy or a shorter time until your next colonoscopy. If your doctor was not able to advance the scope through your entire colon, a barium enema or virtual colonoscopy might be suggested to examine the rest of your colon.
Hill Regional (HRH) Hospital is here to assist all your medical needs with specialists and surgeons trained and experienced in the most advanced treatments. Our highly qualified doctors, nurses, and administrators are dedicated to caring for you with compassion in our state-of-the-art facilities.
Call us on 254-580-8500 to book an appointment with our specialist doctors.